After tissues are removed from cancer patients, pathologists’ role would start intensively giving patients a precise diagnosis and staging as the guide for cancer therapy. In some cancer types, the pathologist would use a biomarker named Ki-67 to tell how rapidly cancer cells divide and how vicious the tumor is. Tumors that produced more Ki-67 tend to grow faster and are more likely to link to poor disease outcome.
Ki-67 have been used to predict disease progression for several different forms of cancers. However, existing knowledge of Ki-67 lies mainly on its role in cell proliferation, the mechanism of how Ki-67 regulates the progression of cancer is still largely unclear.
The group led by Dr.Michael Hsiao of Genomics Research Center spent more than four years in quest for answers. Through a systematic approach combining the analysis of clinical data, cell based experiments, and in vivo animal study, they have come to the conclusion that NIFK, a Ki-67 interacting protein, not only works as a partner with Ki-67 in cancer proliferation but also solely holds responsible for cancer metastasis among non-small cell lung cancer patients. Runx1 is also first identified as a novel protein to participate in NIFK promoted cancer progression. The study has been published on the eLIFE journal lately.
The study is originated from the effort of Dr. Ming-Daw Tsai, who has previously identified the mechanism of the interaction between NIFK and Ki-67 in 2005. With this important molecular mechanism as the foundation, Dr. Hsiao’s team starts to investigate the role of NIFK in cancer.
 |
| Researh team(from left to right): Dr. Tsung-Chieh Lin, Dr. Ming-Daw Tsai, Dr. Michael Hsiao and research assistant Ms. Chia-Yi Su. |
By using the large public database provided by The Cancer Genome Atlas (TCGA) project, they identified the significant correlation between Ki-67 and NIFK in almost all major cancer types, and the strongest association was observed in non-small cell lung cancer. Besides, in lung cancer, NIFK expression level exhibited the strongest prognosis predictive power. Therefore, lung cancer becomes the number one target for NIFK in cancer investigation.
Furthermore, after analyzing cancer tissues from Taiwanese patients by immunohistochemical staining, stronger NIFK expression was seen in non-small cell lung cancer tissue than paired normal lung tissue in the same patient. In Taiwanese cohort, NIFK also had strong prognosis predictive power as seen in public database. Patients with high NIFK expression tumor are more likely to have poor survival outcome and lymphatic metastasis and distant metastasis.
After revealing the critical role of NIFK in non-small cell lung cancer, the team carried out experiments using human cancer cell lines. By regulating NIFK gene expression, they proved that lung cancer cells with higher NIFK expression tend to migrate faster. Similar pattern was confirmed in mice experiments which showed more metastatic nodules in mice injected with high NIFK expression cancer cells. Next step is to answer the question that if Ki-67 participates in NIFK promoted cancer progression.
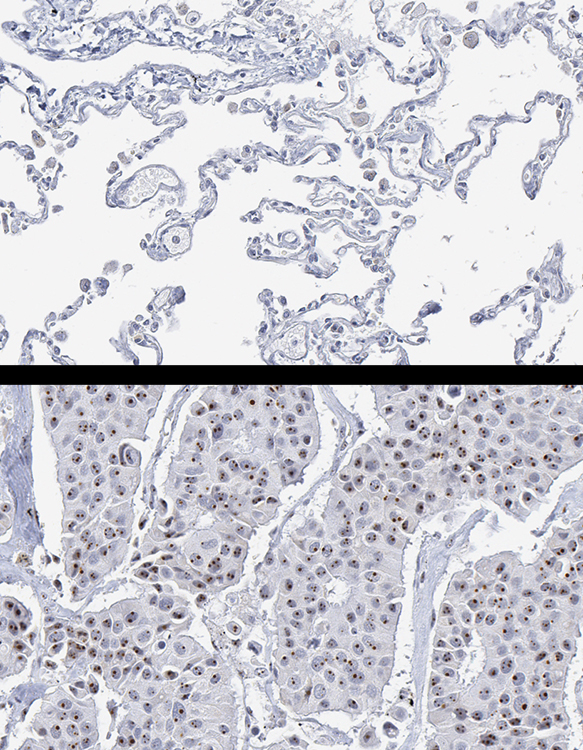 |
| Immunohistochemical (IHC) analysis shows abundant NIFK expression (dark dots) inside nucleoli of lung cancer tissue in the lower diagram as opposed to no NIFK expression in normal lung issue in the upper diagram. This makes NIFK IHC analysis a possible tool for pathological examination. |
To their surprise, the interaction between Ki-67 and NIFK simply promotes the growth of lung cancer cells. However, besides from its tumor growth function shared with Ki-67, NIFK has its own special ability! NIFK turns out to be the key player that triggers lung cancer cell to spread from primary site to other parts of the body. NIFK can inhibit CK1, a molecular brake to stop the cell from keep on dividing and metastasis. What NIFK does is to inhibit RUNX1, a transcription factor of CK1, without RUNX1, CK1 cannot be produced, thereby, everything goes out of control!
“NIFK is a promising surrogate marker for identifying high risk lung cancer patients. Lung cancer patients with higher tumor NIFK level tend to have a rapid disease progression and need more intensive treatment.” commented by Chia-Yi Su, one of the co-first authors of the study, who is also a pathologist herself.
As for the following steps, Dr. Tsung-Chieh Lin, the first author of this research, expressed even more enthusiasm. “The next step is to investigate why and how NIFK is overexpressed in lung cancer patients and whether it plays similar roles in other human cancers. It is also important to develop novel compounds targeting NIFK to see if they can be used in lung cancer treatment. The research works may be hard and difficult. However, they can continue to bring the welfares to human beings.” said Dr. Lin.
This research is the product of tremendous efforts from many groups participated in the study including: Dr. Michael Hsiao’s Laboratory of Genomics Research Center, Dr. Ming-Daw Tsai’s Laboratory of Institute of Biochemistry, Academia Sinica, Dr. Ming-Shyan Huang, Dr. Chih-Jen Yang, Dr. Yu-Peng Liu of Kaohsiung Medical University, Dr. Lu-Ping Ger, Dr. Hong-Tai Chang of Kaohsiung Veterans General Hospital, Dr. Yuan-Feng Lin, Dr. Chi-Long Chen of Taipei Medical University, Dr. Chi-Tai Yeh of Shuang-Ho Hospital, and Dr. John Shyy of University of California at San Diego. The team expressed great appreciation toward the funding supports from Academia Sinica Thematic Grant, SUMMIT Program, and Ministry of Science and Technology.
The full article can be found online at eLIFE website: The nucleolar protein NIFK promotes cancer progression via CK1α/β-catenin in metastasis and Ki-67-dependent cell proliferation.

