A collaborated research led by Dr. Kuo-I Lin of Genomics Research Center has successfully bridged insights of basic research and medical practice, analyzed clinical data from Taiwan and UK, and unveiled the mystery of Ankylosing Spondylitis, a disease that could be making the lives of a significant number of people miserable. Their work was published online in the Journal of Clinical Investigation website early November, 2019. A review regarding their publication was released by Nature Reviews Rheumatologyalso shortly after.
 |
| A review was released by Nature Reviews Rheumatologyalso. |
Ankylosing Spondylitis, commonly referred to as “AS”, is a kind of disease that usually started with the inflammation in the pelvic area, extending to the vertebral column and eventually leading to “bamboo spine”, when patients cannot keep their backs straight up. Statistically, AS happens more on men, and the early symptoms are usually chronic lower back pains at young ages. There is lack of knowledge in what have caused the inflammation, and how exactly the bone like substance starts to accumulate around the vertebra, connecting the ligament to the bone, and causing the inflexibility of the spine eventually.
Dr. Chin-Hsiu Liu, who is the first author of this publication, is also a physician in the Division of Allergy, Immunology and Rheumatology of Taipei Tzu Chi Hospital. Liu was frustrated for not being able to help her AS patients with better cures. She decided to join Professor Kuo-I Lin’s team as a student of Ph.D. Program in Translational Medicine, Kaohsiung Medical University and Academia Sinica seven years ago, aiming to find out a way to cure and help AS patients, despite her already busy physician schedule.
Current treatment of AS circles around blocking inflammation. However, bone like cells may still grow and patients can still develop into bamboo spine status. Therefore, in order to find out the root cause, they need to understand how the bone like cells from patients are formed.
 |
| Team members(from left to right): Dr. Shih-Chieh Hung, Dr. Chin-Hsiu Liu, Dr. In-Ho Chen and Dr. Kuo-I Lin |
It is known that bone cells are generated by mesenchymal stem cells (MSCs). The best way to tackle this question would be to derive MSCs from the patients’ onset lesion. Luckily, through working with Dr. In-Ho Chen of the Hualien Tzu Chi Hospital, they obtained the biopsy after spinal surgeries.
Dr. Shih-Chieh Hung of China Medical University in Taichung and Adjunct Research Fellow at Institute of Biomedical Science (IBMS), Academia Sinica, is an expert in MSC research and the co-corresponding author of this study. They established the MSCs from the biopsy tissues, injected them into immunodeficient mice. By this way, they could observe how human MSCs from patients grow. The result was amazing! After 3 weeks since the injection, they could reproduce formation of the irregular bone like cells on the spines of mice implanted with MSCs from AS patients.
HLA-B27 gene has been known to be associated with AS. It is known that 95% -99% of the AS patients have HLA-B27 gene; yet, no clue whatsoever as why HLA-B27 plays in this ordeal. The team found that, in patient MSCs, HLA-B27 triggered a misfolding protein response, then, a series of abnormal signal transduction took place, and eventually, a gene called TNAP would be highly activated. Elevated TNAP is demonstrated to be the cause of the bone like cell formation. With the animal disease model, they also tested several drugs to see if any can block the new bone formation in mice. Three drugs turned out promising and the team is quite excited.
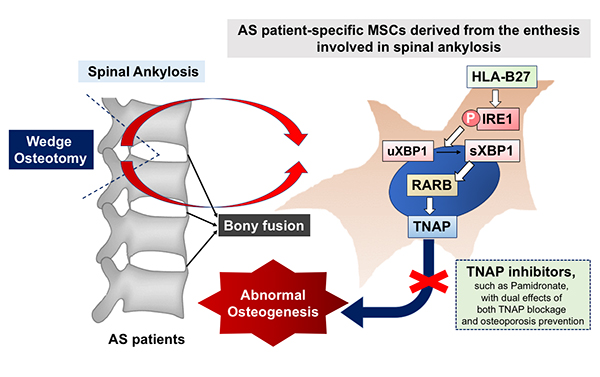 |
| AS patient-specific MSCs derived from the enthesis involved in spinal ankylosis |
Since the overall AS patients in Taiwan is around 100,000, it remains unpredictable which patients will develop “bamboo spine” as disease progresses. The team approached Dr. Sengupta Raj in Royal National Hospital for Rheumatic Diseases in UK. Through the collaboration, they examined the serum samples of both Taiwanese, collected by Dr. Chun-Hsiung Chen from Taipei Tzu Chi Hospital, and British patients. The team found that serm level TNAP, termed BAP, can be a disease progression biomarker in different races.
Dr. Liu pinpointed that micro-trauma could be one of the causes to trigger the abnormal folding of HLA-B27, and there are certainly more worth digging in regard to this topic. The drug “pamidronate” that is being used for treating Osteoporosis is promising, and a formal clinical trial on human should be initiated.
“This is a work with combined effort from a variety of research disciplines, especially from several physicians at different hospitals and different regions. With the pathway unveiled, finding better drugs to treat Ankylosing Spondylitis is more than realistic. We are hoping this study will lead to a new therapy for patients.” Commented Dr. Lin.
The research paper can be read online at: https://jci.org/articles/view/125212
The review article is at: https://www.nature.com/articles/s41584-019-0343-2

