Hepatitis B is a viral infection that attacks the liver. It causes both acute and chronic disease that can lead to liver cirrhosis and liver cancer. Identifying carriers requires a blood test for hepatitis B surface antigen (HBsAg), which must be repeated regularly to ensure virus inactive.
Generally, seroclearance of HBsAg is recognised as the “functional cure” for CHB and confers improved clinical outcomes. However, it is difficult and may even take years to achieve HBsAg decline and seroclearance.
Towards a Functional Cure, there is a great need to investigate promising predictors or novel biomarkers capable of accurately predicting HBsAg seroconversion.
Professor Yang, Hwai-I of Genomics Research Center discovered that soluble programmed death-1 (sPD-1) is a novel immune marker which independently predicts spontaneous HBsAg seroclearance of HBeAg‐negative inactive CHB patients with undetectable HBV DNA. This research has been published in the prestigious journal AP&T Alimentary Pharmacology & Therapeutics.
“It is widely accepted that serum HBsAg levels are the most important predictors of spontaneous HBsAg seroclearance in treatment naïve CHB patients.” said Dr. Yang. “We aimed to identify biomarkers that could predict HBsAg level changes and subsequent seroclearance.”
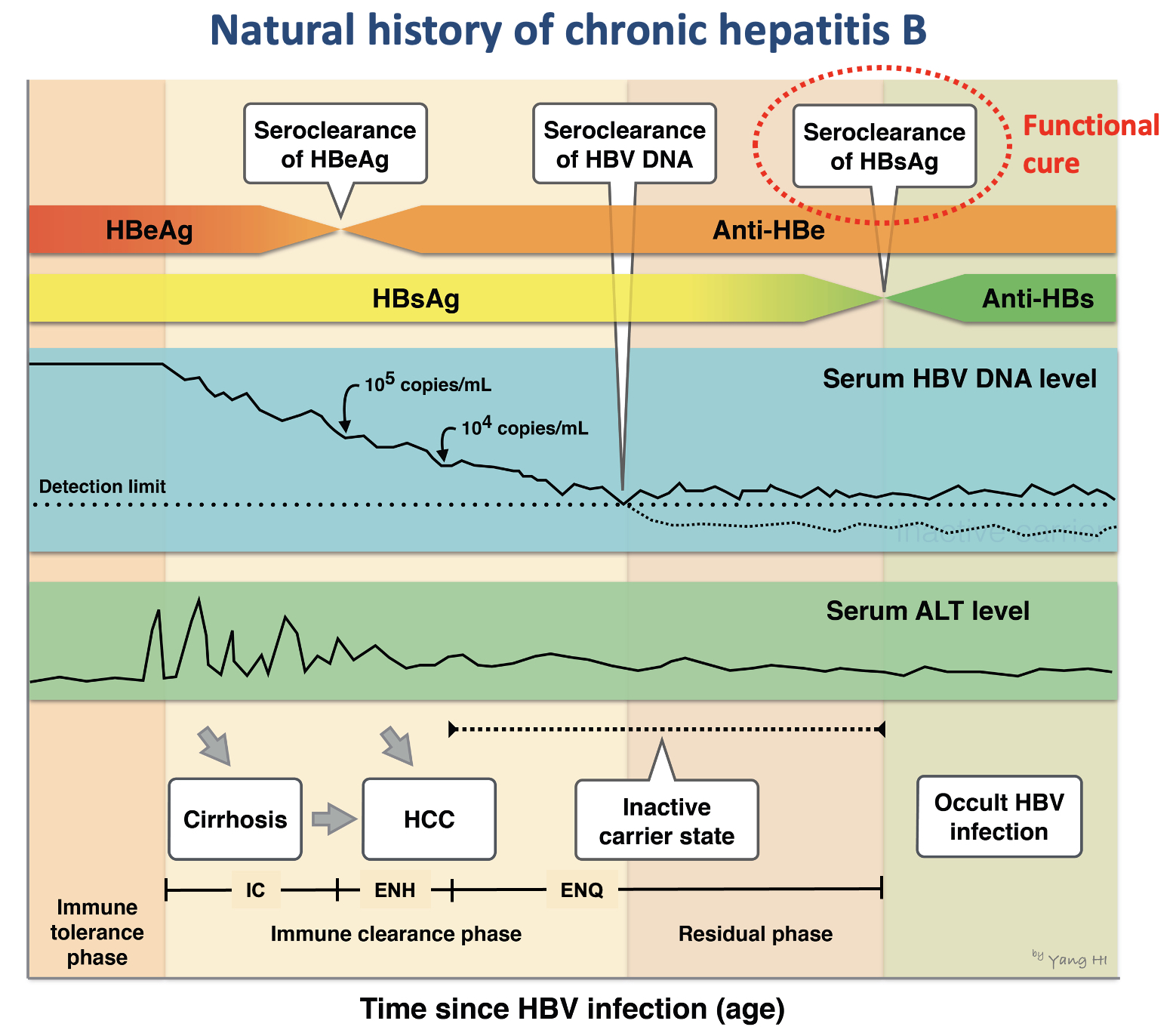
Programmed cell death protein 1 (PD-1), an immunosuppressive molecule expressed in T cells to suppress anticancer immunity, has been shown to be correlated with chronic HBV or HCV infection and HCC development. Upregulation of PD‐1 and PD‐ L1 is associated with T-cell exhaustion and correlated with off‐therapy sustained response.
“Biomarkers nowadays applied for clinical outcome prediction are mainly HBV related. There are limited serum immunological markers available that could reflect host immune response against HBV. Our study focuses on if the immune marker sPD‐1 is associated with HBsAg level changes and predictive of functional cure.” said Dr. Yang.
A total of 1,046 HBeAg seronegative CHB individuals who had undetectable HBV DNA levels, reflecting a low or non-replicating period, were used for analysis in this study. Participants were part of the Risk Evaluation of Viral Load Elevation and Associated Liver Disease/Cancer‐Hepatitis B Virus (REVEAL‐ HBV) cohort, which is led by Dr. Chieh-Jen Chen and Dr. Hwai-I Yang starting from 1991. By recruiting volunteers randomly from 7 townships in Taiwan, they identified 4,155 participants and periodically followed them until 2004.
Among the study subjects, 390 (37.3%) achieved spontaneous HBsAg seroclearance during a mean 5.4 years of follow‐up. sPD‐1 levels at study entry were inversely associated with HBsAg levels measured at the same time as well as with a greater decline in HBsAg levels during follow‐up. Furthermore, cumulative incidences of HBsAg seroclearance by age or follow‐up time increased dramatically with decreasing levels of baseline sPD‐1 in all participants.
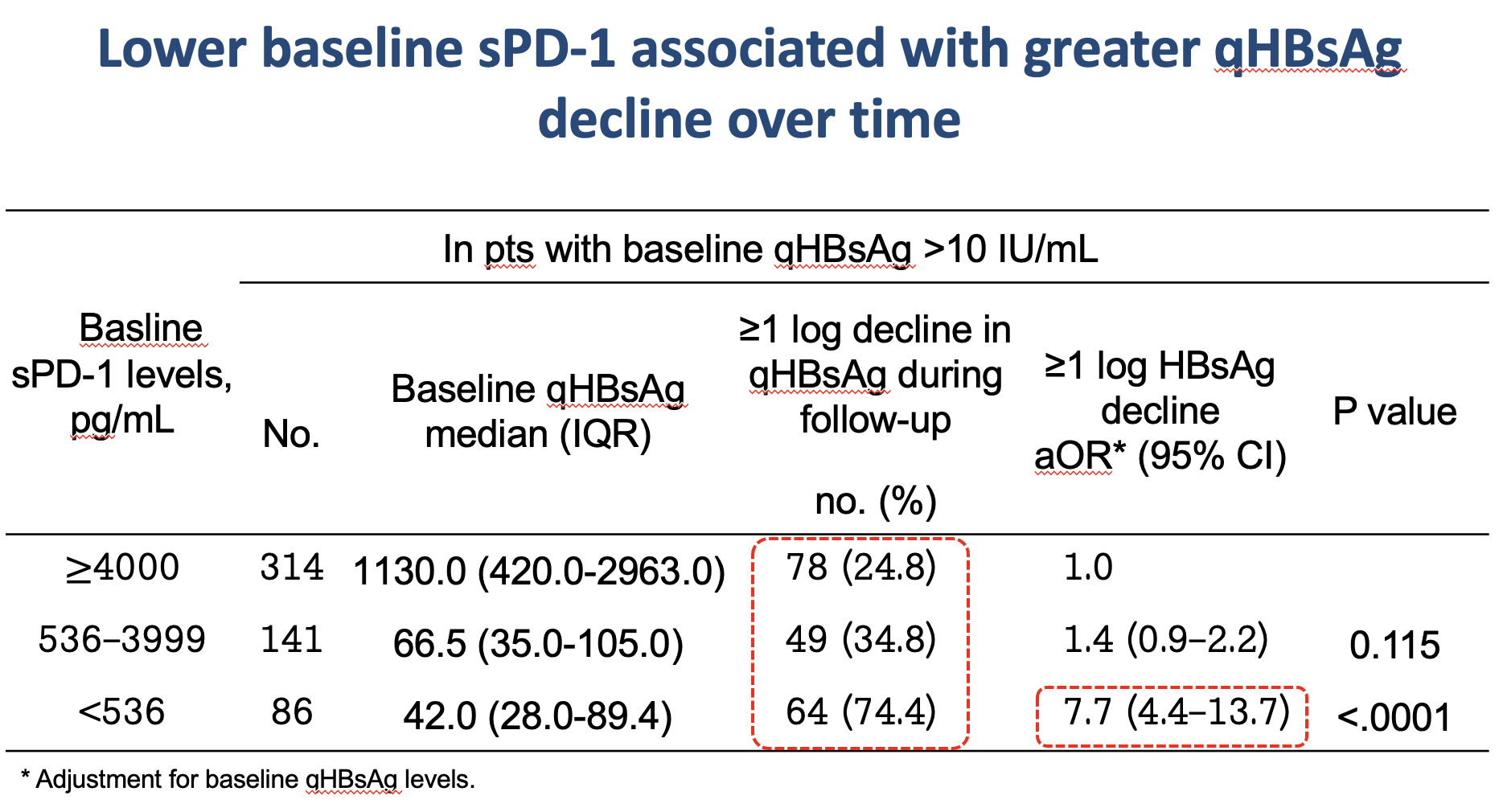
“This is the first study to find out that reduced levels of sPD‐1 predict HBsAg decline and seroclearance in a dose‐dependent manner among HBeAg‐seronegative CHB patients with HBV DNA undetectability, even after adjustment for known predictors” Dr. Yang concluded. “This marker may help identify patients with a higher possibility of achieving HBsAg seroclearance and provide a glimpse into the recovery of host immunity and functional cure.”
The paper titled: “Serum soluble programmed cell death 1 levels predict spontaneous functional cure in inactive carriers with chronic hepatitis B” can be read online at: https://onlinelibrary.wiley.com/doi/full/10.1111/apt.16752

