An accident caused the spinal injury, and a person was sentenced to life time on wheels - such traumatic stories are not new, and all those paralyzed are still waiting for new medical breakthroughs.
That is why one of the toughest remaining mysteries in life science that make scientists pondering upon eagerly is Neuro-regeneration. It is known that some of the damaged nerve cells, or “neurons” to be more exact, can grow back slowly but eventually, like the nerve cells in our limbs; however, there is no such luck for neurons in our spinal cord which are responsible for relaying information from our brains to and from other body parts.
Using a modern day telecommunication as an analogy, the spinal cord is very much like the optical fiber cable that connects all the communication switch points to send data around the world. When there is a “Network out of service” situation due to a backbone damages, it can be a big deal in our lives. The difference is, a broken cable can be replaced, but a damage to the spinal cord is irreversible.
Or, maybe there is a hope, and it is near!
At least, in the experiments conducted by Dr. Shang-Cheng Hung of Genomics Research Center of Aca-demia Sinica, Taiwan, and Dr. Kenji Kadomatsu from School of Medicine of Nagoya University, Japan, they have demonstrated at the cellular level, how CNS neurons broken at the axon section were successfully repaired and regrown. The report of this work has been published in the latest Nature Chemical Biology.
The collaboration started with a spark when the two scientists met at a conference, Dr. Kadomatsu is an established neuroscientist, and Dr. Hung is an established chemist. The spark was “heparan sulfate”(HS), a linear polyanionic polysaccharide that covalently attaches to the proteins on the cell surface, and proved to be effective in the prevention of blood clogging and inhibition of viral and bacterial infection and tumor metastasis, and are being studied for its possible roles in Alzheimer's disease and Parkinson's disease.
HS has a diverse set of biological properties, depending on its number and variation of where the sulfonate groups are constructed. The synthesis of glycan molecules is a challenging task for chemists. Dr. Hung’s team is internationally well-known to prepare the structurally complicated HS saccharides. have special ways to synthesize HS molecules. HS has a chemical structure with eight monosaccharides linked together.
In order to find out that HS sugars has a role in damaged axons, they set the octasaccharides (eight monosaccharides linked together) as the targets and create different sulfation patterns of HS molecules. The Hung’s team spent over quite a long period of time and synthesized 16 different types of HS compounds. Dr. Kadomatsu’s team then tested in-vitro with damaged neurons. They isolated from adult rat dorsal root ganglion (DRG). The lay HS on petri dishes and cut the neurons and put back to observe.
The result was more than inspiring!
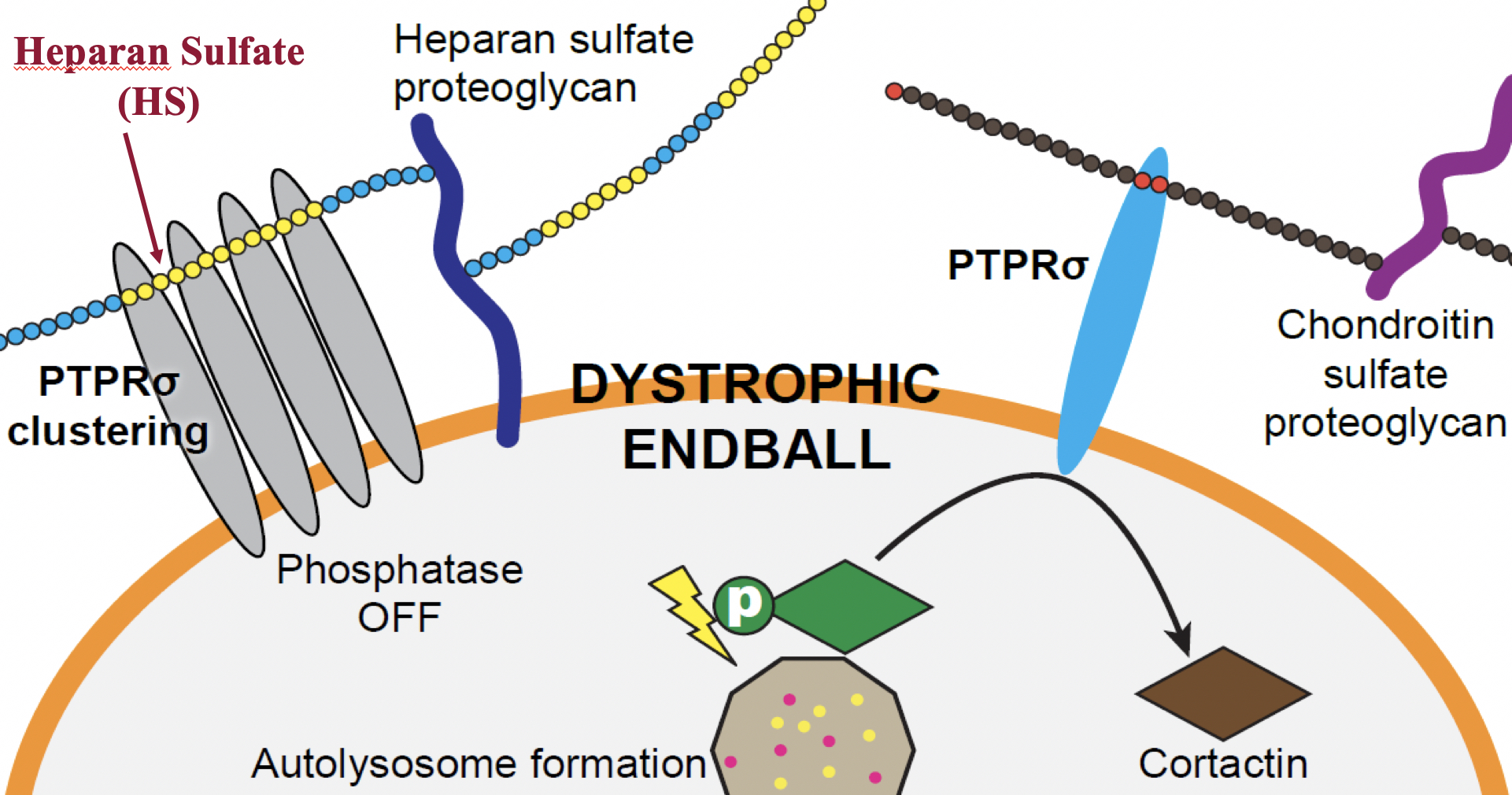
Their study derives a conclusion that, when the spine encountered major impacting forces, out of reasons unknown yet, a substance called Chondroitin Sulfate (CS) will be accumulated at the injury site. CS then binds to a receptor molecule called PTPRσ, and subsequently activated the receptor’s enzymatic activity, and removes the phosphonate group from a molecule called cortactin. The dephosphorylated cortactin appeared to play a major role in stopping the regeneration of axons because it stopped the autophagy and transformed axon tips to ball-like structures, so called dystrophic endballs. The lab verified this by synthesized CS compounds created by Dr. Tamura’s group. HS and CS molecules have similar structure and bind to the same receptor PTPRσ.
|
| Heparan Sulfate bind to PTPRσ's and form clusters to stop the endball effect. |
On the contrary, if the damaged cell is treated with the chemically synthesized HS compounds, in their work, it shows that the higher sulfonated HS octasaccharide is long enough to beat CS and wraps several PTPRσs together to form clusters. Magically, the tamed PTPRσ cluster will no longer trigger any downward dephosphorylation of cortactin, and the axon was given a break to find a way to fix itself.
In a video, the team presented exciting recording of damaged axons keeps growing at full speed at day two when encountering HS molecules in-vitro. They also demonstrated in another video when the growing neurons met CS molecules pre-coated on the dish and formed dystrophic endballs.
Neurons of adult rats cut and enriched with HS regenerated at day 2.
How exciting! However, there is a catch to this excitement! According to Dr. Hung, it took more than 50 steps and months of work to synthesize the HS octasaccharides right now. They would need to work on streamlining the processes.
Nonetheless, the hope to regeneration of spinal axons is stronger than ever! “The findings have provided important molecular targets to cure neuronal injuries. For example, HS oligosaccharides or PTPRσ inhib-itors can be the possible candidates for therapeutics.” Commented Dr. Kazuma Sakamoto, an Associate Professor at the Nagoya University and the co-first authors of this published article.
The team is also excited about the insights they have brought to the mechanism of Parkinson’s disease and Alzheimer disease, because autophagy disruption is often observed in these diseases.
A successful international interdisciplinary collaboration model is also cheered upon. The authors acknowledge the financial support of this study from the Taiwan side: the Ministry of Science and Technology and Academia Sinica; and the Japan side: the Ministry of Education, Culture, Sports, Science and Technology, as well as the Japan Society for the Promotion of Science.
The research report can be read online at: https://www.nature.com/articles/s41589-019-0274-x


